What's in this article?
Cancer of the Uterus Overview
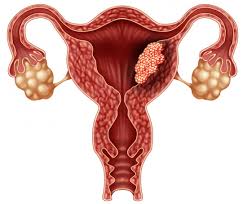
The uterus, or womb, is an important female reproductive organ. It is the place where a baby grows when a women is pregnant. There are different types of uterine cancer. The most common type starts in the endometrium, the lining of the uterus. This type of cancer is sometimes called endometrial cancer.
The symptoms of uterine cancer include
- Unusual vaginal bleeding or discharge
- Trouble urinating
- Pelvic pain
- Pain during intercourse
Uterine cancer usually occurs after menopause. Being obese and taking estrogen-alone hormone replacement therapy (also called menopausal hormone therapy) also increase your risk. Treatment varies depending on your overall health, how advanced the cancer is and whether hormones affect its growth. Treatment is usually a hysterectomy, which is surgery to remove the uterus. The ovaries and fallopian tubes are also removed. Other options include hormone therapy and radiation.
What are the symptoms of uterine cancer?
The most common symptom of uterine cancer is abnormal vaginal bleeding. It may start as a watery, blood-streaked flow that gradually contains more blood. After menopause, any vaginal bleeding is abnormal.
These are common symptoms of uterine cancer:
- Abnormal vaginal bleeding, spotting, or discharge
- Pain or difficulty when emptying the bladder
- Pain during sex
- Pain in the pelvic area
These symptoms may be caused by uterine cancer or by other health problems. Women with these symptoms should tell their doctor so that any problem can be diagnosed and treated as early as possible.
How common is it?
It is estimated that about 2400 women in Australia are diagnosed with uterine cancer each year.1 The majority of uterine cancers are diagnosed in women aged 50 and over. Uterine cancer is the most commonly diagnosed gynaecological cancer in Australia.
What are the risk factors?
The exact cause of cancer of the uterus is unknown, but some factors seem to increase a woman’s risk:
- being aged over 50
- being postmenopausal
- endometrial hyperplasia, a benign condition that occurs when the endometrium grows too thick
- never having children or being infertile
- starting periods early (before age 12)
- reaching menopause late (after age 55)
- having high blood pressure (hypertension)
- having diabetes
- being overweight or obese
- a family history of ovarian, uterine, breast or bowel cancer
- previous ovarian tumours, or polycystic ovary syndrome
- taking oestrogen hormone replacement without progesterone
- previous pelvic radiation for cancer
- taking tamoxifen to treat breast cancer. The risk of uterine cancer is usually outweighed by the benefits of treating breast cancer. Talk to your doctor if you are concerned.
Many women who have risk factors don’t develop cancer of the uterus, and some women who do get cancer have no risk factors.
What types are there?
Uterine cancer can be either endometrial cancer or the less common uterine sarcoma.
Endometrial cancers
Most cancers of the uterus begin in the lining of the uterus and are called endometrial cancers. There are two main types of endometrial cancer:
| Type 1 cancers | Usually called endometrioid cancers. Type 1 cancers are the most common types of endometrial cancer and usually require less intensive treatment. |
| Type 2 cancers | Include malignant mixed Müllerian tumours, serous carcinoma and clear cell carcinoma. Type 2 cancers are much less common types of endometrial cancer. Treatment usually involves more invasive surgery and chemotherapy and/or radiotherapy. |
Uterine sarcomas
These develop in the muscle of the uterus (myometrium) or the connective tissue supporting the endometrium, which is called the stroma. There are three types:
|
These types are rare and may be more likely to spread to other parts of the body. |
What are the treatment of uterine cancer?
Treatment options for people with uterine cancer are surgery, radiation therapy, chemotherapy, and hormone therapy. You may receive more than one type of treatment.
The treatment that’s right for you depends mainly on the following:
- Whether the tumor has invaded the muscle layer of the uterus
- Whether the tumor has invaded tissues outside the uterus
- Whether the tumor has spread to other parts of the body
- The grade of the tumor
- Your age and general health
You may have a team of specialists to help plan your treatment. Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat uterine cancer include gynecologists, gynecologic oncologists (doctors who specialize in treating female cancers), medical oncologists, and radiation oncologists. Your health care team may also include an oncology nurse and a registered dietitian.
Your health care team can describe your treatment choices, the expected results of each, and the possible side effects. Because cancer therapy often damages healthy cells and tissues, side effects are common. Before treatment starts, ask your health care team about possible side effects and how treatment may change your normal activities. You and your health care team can work together to develop a treatment plan that meets your needs.
At any stage of disease, supportive care is available to control pain and other symptoms, to relieve the side effects of treatment, and to ease emotional concerns. Information about such care is available on NCI’s Web site at http://www.cancer.gov/cancertopics/coping.
Also, NCI’s Cancer Information Service can answer your questions about supportive care. Call 1–800–4–CANCER (1–800–422–6237). Or chat using LiveHelp, NCI’s instant messaging service, at https://livehelp.cancer.gov/app/chat/chat_launch.