Achalasia is a rare disease of the muscle of the esophagus (swallowing tube). Achalasia is a condition that affects the esophagus, the tube that carries food from the throat to the stomach. In individuals with achalasia, the esophagus does not work properly. Food may become trapped in it.
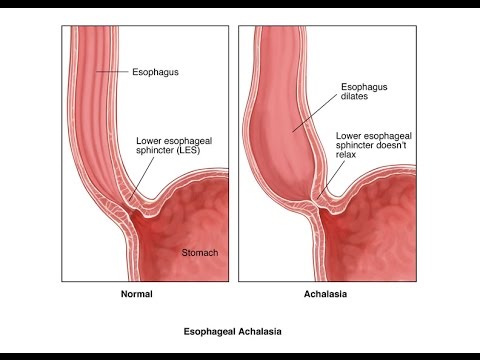
This condition can be related to damage to nerves in the esophagus. It can also be caused by damage to the lower esophageal sphincter. The lower esophageal sphincter is a valve that closes off the esophagus from the stomach.
Achalasia is characterized by difficulty in swallowing, regurgitation, and sometimes chest pain.
Achalasia is rare. It may occur at any age, but is most common in middle-aged or older adults. The problem may be inherited in some people.
Causes
Achalasia can happen for different reasons. It can be difficult for doctors to point out specific causes. This condition may be hereditary, or it may be caused by an autoimmune condition, where the body attacks itself. Degeneration of nerves in the esophagus often contributes to the advanced symptoms of the condition.
Other conditions can cause symptoms similar to achalasia. Cancer of the esophagus is one of these conditions. Another is a rare parasitic infection called Chagas disease.
Symptoms
- Backflow (regurgitation) of food
- Chest pain, which may increase after eating or may be felt in the back, neck, and arms
- Cough
- Difficulty swallowing liquids and solids
- Heartburn
- Unintentional weight loss
Diagnosis
Doctors often suspect achalasia in patients who have trouble swallowing both solids and liquids, particularly when this problem gets worse over time.
To diagnose achalasia, doctors may use esophageal manometry. This involves having a tube placed in your esophagus while you swallow. The tube records the muscle activity and makes certain everything is working correctly. An X-ray, or similar exam, of your esophagus may also be used to diagnose this condition. Other doctors prefer to perform an endoscopy. In this procedure, a small camera is put into the esophagus to look for problems.
Treatment
Treatments for achalasia include oral medications, stretching of the lower esophageal sphincter (dilation), surgery to cut the sphincter (esophagomyotomy), and the injection of botulinum toxin (Botox) into the sphincter. All four treatments reduce the pressure within the lower esophageal sphincter to allow easier passage of food from the esophagus into the stomach.
Oral medications
Oral medications that help to relax the lower esophageal sphincter include groups of drugs called nitrates, for example, isosorbide dinitrate (Isordil) and calcium channel blockers, for example, nifedipine (Procardia) and verapamil (Calan). Although some patients with achalasia, particularly early in the disease, have improvement of symptoms with medications, most do not. By themselves, oral medications are likely to provide only short-term and not long-term relief of the symptoms of achalasia, and many patients experience side-effects from the medications.
Dilation
The lower esophageal sphincter also may be treated directly by forceful dilation. Dilation of the lower esophageal sphincter is done by having the patient swallow a tube with a balloon at the end. The balloon is placed across the lower sphincter with the help of X-rays, and the balloon is blown up suddenly. The goal is to stretch–actually to tear–the sphincter. The success of forceful dilation has been reported to be between 60% and 95%. Patients in whom dilation is not successful can undergo further dilations, but the rate of success decreases with each additional dilation. If dilation is not successful, the sphincter may still be treated surgically. The main complication of forceful dilation is rupture of the esophagus, which occurs 5% of the time. Half of the ruptures heal without surgery, though patients with rupture who do not require surgery should be followed closely and treated with antibiotics. The other half of ruptures require surgery. (Although surgery carries additional risk for the patient, surgery can repair the rupture as well as permanently treat the achalasia with esophagomyotomy.) Death following forceful dilation is rare. Dilation is a quick and inexpensive procedure compared with surgery, and requires only a short hospital stay.
Esophagomyotomy
The sphincter also can be cut surgically, a procedure called esophagomyotomy. The surgery can be done using an abdominal incision or laparoscopically through small punctures in the abdomen. In general, the laparoscopic approach is used with uncomplicated achalasia. Alternatively, the surgery can be done with a large incision or laparoscopically through the chest. Esophagomyotomy is more successful than forceful dilation, probably because the pressure in the lower sphincter is reduced to a greater extent and more reliably; 80%-90% of patients have good results. With prolonged follow-up, however, some patients develop recurrent dysphagia. Thus, esophagomyotomy does not guarantee a permanent cure. The most important side effect from the more reliable and greater reduction in pressure with esophagomyotomy, is reflux of acid (gastroesophageal reflux disease or GERD). In order to prevent this, the esophagomyotomy can be modified so that it doesn’t completely cut the sphincter or the esophagomyotomy may be combined with anti-reflux surgery (fundoplication). Whichever surgical procedure is done, some physicians recommend life-long treatment with oral medications for acid reflux. Others recommend 24 hour esophageal acid testing with lifelong medication only if acid reflux is found.
Botulinum toxin
Another treatment for achalasia is the endoscopic injection of botulinum toxin into the lower sphincter to weaken it. Injection is quick, nonsurgical, and requires no hospitalization. Treatment with botulinum toxin is safe, but the effects on the sphincter often last only for months, and additional injections with botulinum toxin may be necessary. Injection is a good option for patients who are very elderly or are at high risk for surgery, for example, patients with severe heart or lung disease. It also allows patients who have lost substantial weight to eat and improve their nutritional status prior to “permanent” treatment with surgery. This may reduce post-surgical complications.
Prognosis
Prognosis for this condition varies. Some people only have very mild symptoms. For others, treatment can be highly successful. Sometimes multiple treatments are needed to handle symptoms.
Unfortunately, if a dilation procedure doesn’t work the first time, surgery may be needed. Usually, the chance of success decreases with each successive dilation. Therefore, doctors will often seek alternatives if several dilations are not successful.
The success rate for esophagomyotomy is thought to be 80-90%. However, patients may develop some complications. These include:
- issues related to tearing of the esophagus
- acid reflux
- respiratory conditions caused by food travelling up the esophagus and into the windpipe