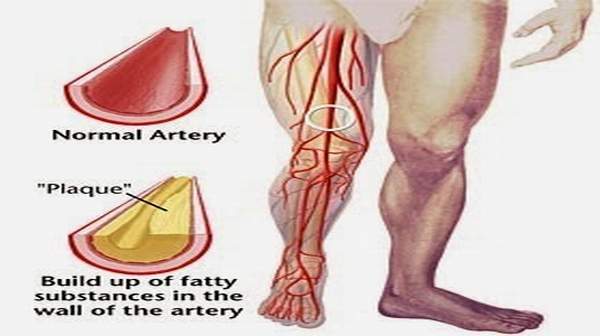
Blood vessel disease is also called Peripheral Vascular Disease (PVD) or artery disease. It is the narrowing of the blood vessels in the abdomen, legs and arms. Blood vessel disease is caused by a build-up of fatty deposits called plaque that narrows blood vessels. When the blood vessels narrow, less oxygen-rich blood gets to your body parts. This can cause tissue and cell death. Blood vessel disease is the leading cause of amputations.
Types of PVD
There are two main types of PVD:
- Functional PVD: This does not involve physical problems in the blood vessels. It causes incidental or short-term symptoms. These are usually spasms that occur erratically.
- Organic PVD: This involves changes in blood vessel structure. This type of PVD causes inflammation, tissue damage, and blockages.
Causes
Functional PVD
The body responds to certain external stimuli by restricting blood flow to the peripheral vessels. The most common causes of functional PVDs are:
- emotional stress
- smoking
- cold temperatures
- operating vibrating machinery or tools
Physical changes can affect the structure of blood vessels. For example, arteriosclerosis can cause plaque buildup. The primary causes of such organic
- smoking
- high blood pressure
- diabetes
- high cholesterol
Additional causes of organic PVDs include:
- injury to extremities
- muscles or ligaments with abnormal structures
- infection
- coronary artery disease
- Muscle pain, aches or cramps
- Cool, pale skin, cold hands and feet
- Reddish-blue color of the skin and nails of the hands and feet
- A sore that takes a long time to heal or when scabbed over, looks
- black
- Loss of hair on legs, feet or toes
- Faint or no pulse in the legs or feet
- Pain with exercise that goes away when you rest
If you have any of the signs, call your doctor to get checked.
For many people, there are no symptoms of PVD. For others, the first signs of PVD begin slowly and irregularly. You may feel discomfort in your legs and feet. You may experience:
- painful cramping
- achiness
- fatigue
- burning
Typically, you will feel these sensations when you walk. You may first notice them when walking quicker, with more exertion, or for long distances. The pain will intensify with activity and subside when you rest. This is called intermittent claudication.
Intermittent claudication occurs because your muscles need more blood flow during activity. In PVD, the vessels are narrowed with plaque. They can only supply a limited amount of blood. This causes more problems during activity than at rest. Lack of blood causes pain and discomfort.
As your PVD progresses, symptoms will occur more frequently. It will require less exertion to bring them on. Eventually, you will experience leg pain and fatigue even at rest.
Additional symptoms may occur as a result of reduced blood supply. With PVD, you may have:
- skin changes on your legs and feet (thinning, , shiny, or paleness may occur)
- weak pulses in your legs and feet
- gangrene tissue death caused by lack of blood flow
- wounds or ulcers on the legs and feet that won’t heal
- reduced hair growth on your legs
- toes that turn blue
- severe burning pain in your toes
- leg cramps and pain when you are lying in bed
- muscles that feel numb or heavy
- arms and legs that are reddish blue
- toenails that are thick and opaque
It is important to tell your doctor if you experience any symptoms of PVD. Do not assume that the symptoms are simply the results of aging. Delaying diagnosis and treatment could allow the disease to progress further.
Risk Factors
You are at higher risk for blood vessel disease if you:
- Smoke
- Have diabetes
- Are over the age of 45
- Have high cholesterol
- Have high blood pressure Page 2
- Have a family member with heart or blood vessel disease
- Are overweight
- Are inactive
If you have any of the classic symptoms of PVD, it is important to tell your doctor. Early diagnosis is crucial to successful treatment. It can prevent life-threatening complications, such as heart attack and stroke.
To diagnose PVD, your physician will begin with a complete medical history and physical exam. Several tests may be used to diagnose PVD. They are:
- measuring the pulses in your legs and feet—Your physician can check the pulses in your legs and feet with a stethoscope. A whooshing sound called a bruit indicates a narrowed area in the vessel.
- Doppler ultrasound—This test shows the blood flow in your vessels. Ultrasound is not invasive. It uses sound waves to take images.
- ankle-brachial index (ABI)—This is the most common test used to diagnose PVD. A blood pressure cuff and ultrasound assess blood pressure and flow. The blood pressure in your ankle is compared to the blood pressure in your arm. In some cases, readings will be taken before and after you walk on a treadmill. This helps demonstrate how the arteries react to exercise.
- pulse volume recording (PVR)—This test checks the blood flow in your legs. Blood pressure cuffs are wrapped around one arm and leg as you are lying down. The cuffs are inflated slightly. As blood flows through the arteries, a device records the ability of the vessels to expand.
- Angiography—A catheter is guided through an artery in your groin. It is passed to the targeted area. Contrast dye is injected. An X-ray can then diagnose the clogged artery. By inflating a balloon at the end of the catheter, the artery can be opened in the same procedure.
- magnetic resonance angiography (MRA) and computerized tomography angiography (CTA)—These are noninvasive imaging techniques that allow doctors to view blood flow and diagnose blockages.
There are two main goals of PVD treatment. The first is to control pain and symptoms. This allows you to remain active. The second is to stop the disease from progressing. This will lower your risk of serious and life-threatening complications.
Treatment options may include:
- Medications – to help treat atherosclerosis, such as statins to lower LDL cholesterol and antihypertensive drugs to lower blood pressure.
- Drugs to treat blood clots – treatment may include various medications (including anticoagulants and anti-platelet drugs) to prevent blood clots from developing and medications (including thrombolytics) that dissolve existing blood clots.
- Angioplasty – this procedure, usually performed under sedation and local anaesthetic, involves threading a thin tube (catheter) into the narrowed blood vessel through a small incision, usually in the leg. Once the catheter reaches the narrowed or blocked site, the small balloon on its tip is inflated. This widens the blood vessel and improves blood flow. Angioplasty is usually considered as a temporary measure.
- Surgical insertion of a stent – a stent is a metal ‘sleeve’ that is implanted inside the narrowed blood vessel during an angioplasty procedure to prop it open. Stents may be impregnated with medications that help to prevent scar tissue from narrowing the treated area of blood vessel.
- Atherectomy – this operation involves cutting away the fatty obstruction with a small scalpel-like instrument.
- Bypass surgery – this operation is usually only considered in severe cases that don’t respond to other treatments or in cases that involve large sections of the diseased blood vessel. A section of healthy vein is taken from somewhere else in the body and surgically grafted to re-route blood flow around the blockage in the affected blood vessel. A surgeon may sometimes use a piece of synthetic tubing to detour blood flow.
Lifestyle changes are an important part of treatment. Be guided by your doctor, but general self-help suggestions include:
- Take steps to properly manage risk factors, such as diabetes or high blood pressure, as advised by your doctor.
- Quit smoking.
- Exercise regularly. Ask your doctor for advice on appropriate activities.
- Eat a low-fat, high-fibre diet.
- Maintain a healthy weight for your height and build.
- Take care of injuries to the affected area, for example, dress wounds promptly and seek medical attention.
- Take all medications strictly as prescribed.
- See your doctor for regular check-ups.
- See your doctor if you have symptoms in the affected body part such as redness, warmth and swelling. These symptoms could be signs of infection. Treatment may include antibiotics.
You can reduce your risk of developing PVD by having a healthy lifestyle. This includes:
- avoiding smoking
- controlling your blood sugar, if you have diabetes
- setting an exercise goal of 30 minutes a day, three times a week
- working to lower cholesterol and blood pressure
- eating a healthy diet that is low in saturated fat
- keeping your weight at a healthy level
If you experience symptoms of PVD, talk to your doctor. Your doctor may also recommend testing if you are at risk for the disease.
Early diagnosis and treatment can keep symptoms to a minimum. They can also increase the effectiveness of your treatment.
Prognosis
If diagnosed early, most cases of PVD will respond to lifestyle treatments. One way to measure improvement is to determine how far you can walk without pain. With effective treatment, you should be able to gradually increase the distance.