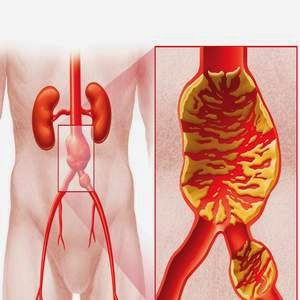
The aorta is the largest artery in your body, and it carries oxygen-rich blood pumped out of, or away from, your heart. Your aorta runs through your chest, where it is called the thoracic aorta. When it reaches your abdomen, it is called the abdominal aorta. The abdominal aorta supplies blood to the lower part of the body. In the abdomen, just below the navel, the aorta splits into two branches, called the iliac arteries, which carry blood into each leg.
An abdominal aortic aneurysm is a dilation (ballooning) of part of the aorta that is within the abdomen. An abdominal aorticaneurysm (AAA) usually causes no symptoms unless it ruptures (bursts). A ruptured AAA is often fatal. An AAA less than 55 mm wide has a low chance of rupture. An operation to repair the aneurysm may be advised if it is larger than 55 mm, as above this size the risk of rupture increases significantly. Men aged 65 and over are to be offered a routine scan to screen for AAA.
Depending on the size and rate at which your abdominal aortic aneurysm is growing, treatment may vary from watchful waiting to emergency surgery. Once an abdominal aortic aneurysm is found, doctors will closely monitor it so that surgery can be planned if it’s necessary. Emergency surgery for a ruptured abdominal aortic aneurysm can be risky.
Causes
The exact causes of the degenerative process remain unclear. There are, however, some hypotheses and well-defined risk factors.
- Tobacco smoking: Greater than 90% of people who develop a AAA have smoked at some point in their life.
- Alcohol and hypertension: The inflammation caused by prolonged use of alcohol and hypertensive effects from abdominal edema which leads to hemorrhoids, esophageal varices, and other conditions, is also considered a long-term cause of AAA.
- Genetic influences: The influence of genetic factors is high. AAA is 4-6 times more common in male siblings of known patients, with a risk of 20-30%. The high familial prevalence rate is most notable in male individuals. There are many hypotheses about the exact genetic disorder that could cause higher incidence of AAA among male members of the affected families. Some presumed that the influence of alpha 1-antitrypsin deficiency could be crucial, while other experimental works favored the hypothesis of X-linked mutation, which would explain the lower incidence in heterozygous females. Other hypotheses of genetic etiology have also been formulated. Connective tissue disorders, such as Marfan syndrome and Ehlers-Danlos syndrome, have also been strongly associated with AAA. Both relapsing polychondritis and pseudoxanthoma elasticum may cause abdominal aortic aneurysm.
- Atherosclerosis: The AAA was long considered to be caused by atherosclerosis, because the walls of the AAA are frequently affected heavily. However, this hypothesis cannot be used to explain the initial defect and the development of occlusion, which is observed in the process.
- Other causes of the development of AAA include: infection, trauma, arteritis, cystic medial necrosis (m. Erdheim).
Symptoms
Abdominal aortic aneurysms often grow slowly and usually without symptoms, making them difficult to detect. Some aneurysms will never rupture. Many start small and stay small, although many expand over time. Others expand quickly. Predicting how fast an abdominal aortic aneurysm may enlarge is difficult.
As an abdominal aortic aneurysm enlarges, some people may notice:
- A pulsating feeling near the navel
- Deep, constant pain in your abdomen or on the side of your abdomen
- Back pain
Tears in the wall of the aorta (dissection) are the main complications of abdominal aortic aneurysm. A ruptured aortic aneurysm can lead to life-threatening internal bleeding. In general, the larger the aneurysm, the greater the risk of rupture.
Signs and symptoms that your aortic aneurysm has burst include:
- Sudden, intense and persistent abdominal or back pain
- Pain that radiates to your back or legs
- Sweatiness
- Clamminess
- Dizziness
- Nausea
- Vomiting
- Low blood pressure
- Fast pulse
- Loss of consciousness
- Shortness of breath
Another complication of aortic aneurysms is the risk of blood clots. Small blood clots can develop in the area of the aortic aneurysm. If a blood clot breaks loose from the inside wall of an aneurysm and blocks a blood vessel elsewhere in your body, it can cause pain or block the blood flow to the legs, toes, kidneys or abdominal organs.
Your doctor will examine your abdomen and feel the pulses in your legs. The doctor may find:
- A lump (mass) in the abdomen
- Pulsating sensation in the abdomen
- Stiff or rigid abdomen
You may have an abdominal aortic aneurysm that is not causing any symptoms. Your doctor may find this problem by doing the following tests:
- Ultrasound of the abdomen when the abdominal aneurysm is first suspected
- CT scan of the abdomen to confirm the size of the aneurysm
- CTA (computed tomographic angiogram) to help with surgical planning
Any one of these tests may be done when you’re having symptoms.
Treatment
Here are the general guidelines for treating abdominal aortic aneurysms.
- Open-abdominal surgery to repair an abdominal aortic aneurysm involves removing the damaged section of the aorta and replacing it with a synthetic tube (graft), which is sewn into place, through an open-abdominal approach. With this type of surgery, it will likely take you a month or more to fully recover.
- Endovascular surgery is a less invasive procedure sometimes used to repair an aneurysm. Doctors attach a synthetic graft to the end of a thin tube (catheter) that’s inserted through an artery in your leg and threaded up into your aorta. The graft — a woven tube covered by a metal mesh support — is placed at the site of the aneurysm and fastened in place with small hooks or pins. The graft reinforces the weakened section of the aorta to prevent rupture of the aneurysm.
Prevention
- Eat a heart-healthy diet, exercise, stop smoking (if you smoke), and reduce stress.
- If you have high blood pressure or diabetes, take your medicines as your doctor has told you.
- Get regular exercise.
- Reduce cholesterol and fat in your diet.
Prognosis