Congestive heart failure (CHF) occurs when the heart isn’t able to pump blood normally. As a result, there is not enough blood flow to provide the body’s organs with oxygen and nutrients. The term “heart failure” does not mean that the heart stops beating completely, but that the heart is not working as efficiently.
CHF affects over 6 million people in North America and is the most common cause of hospitalization for people over 65 years of age. Each year CHF is implicated in over 300,000 deaths.
Men are slightly more at risk than women. People of African descent are considerably more at risk than those of European descent and also have a higher risk of death.
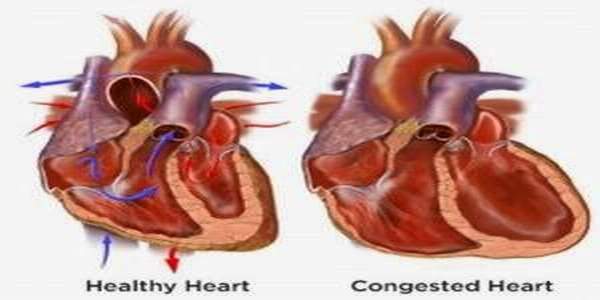
There are two basic problems in congestive heart failure:
- systolic dysfunction – occurs when the heart can’t pump enough blood to supply all the body’s needs
- diastolic dysfunction – occurs when the heart cannot accept all the blood being sent to it
Causes
Heart failure usually develops slowly after an injury to the heart. Some injuries may include a heart attack, too much strain on the heart due to years of untreated high blood pressure, or a diseased heart valve.
- Coronary artery disease
- Previous heart attack (myocardial infarction)
- High blood pressure (hypertension)
- Valve disease
- Congenital heart disease (condition you are born with)
- Cardiomyopathy (enlarged heart)
- Endocarditis
- Myocarditis (infection of the heart)
- Diabetes
- Exertional dyspnea and/or dyspnea at rest
- Orthopnea
- Acute pulmonary edema
- Chest pain/pressure and palpitations
- Tachycardia
- Fatigue and weakness
- Nocturia and oliguria
- Anorexia, weight loss, nausea
- Exophthalmos and/or visible pulsation of eyes
- Distention of neck veins
- Weak, rapid, and thready pulse
- Rales, wheezing
- S3 gallop and/or pulsus alternans
- Increased intensity of P2 heart sound
- Hepatojugular reflux
- Ascites, hepatomegaly, and/or anasarca
- Central or peripheral cyanosis, pallor
- High blood pressure (hypertension)
- Heart attack (myocardial infarction)
- Abnormal heart valves
- Enlargement of the heart (cardiomyopathy)
- Family history of heart disease
- Diabetes
- magnetic resonance imaging (MRI), which takes pictures of your heart
- stress tests to see how well your heart performs under different levels of stress
- blood tests to check for abnormal blood cells and infections
- medicines – such as diuretics (to remove excess fluid), ACE inhibitors (to open up blood vessels, reduce blood pressure and reduce sodium retention and water retention), digitalis (to help the heart pump more effectively), vasodilators (to open up blood vessels) and certain beta-blockers (to slow the heart rate and reduce its work)
- addressing the underlying disorder – for example, treatment of high blood pressure
- lifestyle changes – such as regular gentle physical activity, losing excess body fat, stopping smoking, adhering to a low-fat and low-salt diet, restricting alcohol and having adequate rest
- surgery – to replace narrowed or leaking heart valves
- coronary bypass surgery – in some cases
- heart transplant – in extreme cases.
- Don’t smoke.
- Consume no more than two alcoholic beverages a day.
- Eat a healthy, balanced diet low in salt and fat, exercise regularly and lose weight if you are overweight.
- Adhere to a prescribed treatment program for other forms of heart disease.
- If you are diabetic, maintain careful control of your blood sugar.